"Discount trimox uk, antimicrobial spray".
By: D. Elber, M.B. B.A.O., M.B.B.Ch., Ph.D.
Co-Director, David Geffen School of Medicine at UCLA
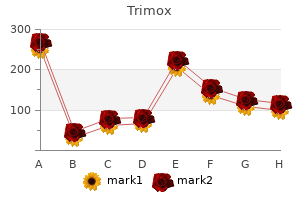
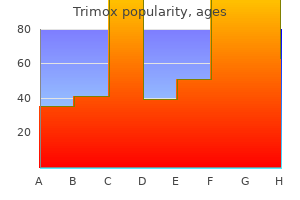
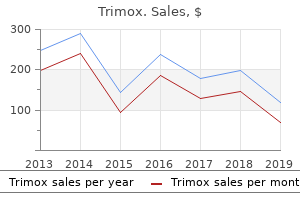
However antibiotics for acne alternatives discount trimox, when the scan does not give the cause antimicrobial yarn suppliers trimox 500mg mastercard, there is no simple solution; usually no single laboratory test or screening procedure will sift out the critical initial diagnostic categories as effectively as a careful clinical evaluation. If the cause of coma is structural, it generally is due to a focal injury along the course of the neural pathways that generate and maintain a normal waking brain. Therefore, the clinical diagnosis of structural coma depends on the recognition of the signs of injury to structures that accompany the arousal pathways through the brain. Structural processes that impair the function of the arousal system fall into two categories: (1) supratentorial mass lesions, which may compress deep diencephalic structures and hence impair the function of both hemispheres, and (2) infratentorial mass or destructive lesions, which directly damage the arousal system at its source in the upper brainstem. The remainder of Chapter 1 will systematically examine the major arousal systems in the brain and the physiology and pathophysiology of consciousness. Chapter 2 addresses examination of the patient with a disturbance of consciousness, particularly those components of the examination that assay the function of the arousal systems and the major sensory, motor, and autonomic systems that accompany them. Once the examination is completed, the examiner should be able to determine whether the source of the impairment of consciousness is caused by a structural lesion (Chapters 3 and 4) or a diffuse and therefore presumably metabolic process (Chapter 5). Although it is important to question family members or attendants who may have details of the history, including emergency medical personnel who bring the patient into the emergency department, the history for comatose patients is often scant or absent. The neurologic examination of a patient with impaired consciousness, fortunately, is brief, because the patient cannot detect sensory stimuli or provide voluntary motor responses. The key components of the examination, which can be completed by a skillful physician in just a few minutes, include (1) the level of consciousness of the patient, (2) the pattern of breathing, (3) the size and reactivity of the pupils, (4) the eye movements and oculovestibular responses, and (5) the skeletal motor responses. From this information, the examiner must be able to reconstruct the type of the lesion and move swiftly to lifesaving measures. Before reviewing the components of the coma examination in detail, however, it is necessary to understand the basic pathways in the brain that sustain wakeful, conscious behavior. Only from this perspective is it possible to understand how the components of the coma examination test pathways that are intertwined with those that maintain consciousness. He was brought up in Austrian Trieste, studied medicine in Vienna, and in 1906 took a post in the Psychiatric Clinic under Professor Julius von Wagner-Jauregg. In 1916 during World War I, he began seeing cases of a new and previously unrecorded type of encephalitis and published his first report of this illness in 1917. Although subsequent accounts have often confused this illness with the epidemic of influenza that swept through Europe and then the rest of the world during World War I, von Economo was quite clear that encephalitis lethargica was not associated with respiratory symptoms, and that its appearance preceded the onset of the latter epidemic. Von Economo continued to write and lecture about this experience for the remainder of his life, until his premature death in 1931 from heart disease. Based on his clinical observations, von Economo proposed a dual center theory for regulation of sleep and wakefulness: a waking influence arising from the upper brainstem and passing through the gray matter surrounding the cerebral aqueduct and the posterior third ventricle; and a rostral hypothalamic sleeppromoting area. These observations became the basis for lesion studies done by Ranson in 1939,20 by Nauta in 1946,21 and by Swett and Hobson in 1968,22 in which they showed that the posterior lateral hypothalamic lesions in monkeys, rats, and cats could reproduce the prolonged sleepiness that von Economo had observed. The rostral hypothalamic sleep-promoting area was confirmed experimentally in rats by Nauta in 194621 and in cats by Sterman and Clemente in the 1960s. A photograph of Baron Constantin von Economo, and excerpts from the title page of his lecture on the localization of sleep and wake promoting systems in the brain. These individuals would develop episodes of sleep attacks during which they had an overwhelming need to sleep. He noted that they also had attacks of cataplexy in which they lost all muscle tone, often when excited emotionally. Von Economo noted accurately that these symptoms were similar to the rare condition previously identified by Gelinaux as narcolepsy. Wilson even described examining a patient in his office, with the young house officer McDonald Critchley, and that the patient indeed had atonic paralysis, with loss of tendon reflexes and an extensor plantar response during the attack. A corollary was that consciousness could only be eliminated by lesions that simultaneously damaged both cerebral hemispheres. The nascent field of neurosurgery also began to contribute cases in which loss of consciousness was associated with lesions confined to the upper brainstem or caudal diencephalon. However, the most convincing body of evidence was assembled by Baron Constantin von Economo,19 a Viennese neurologist who recorded his observations during an epidemic of a unique disorder, encephalitis lethargica, that occurred in the years surrounding World War I. Most victims of encephalitis lethargica were very sleepy, spending 20 or more hours per day asleep, and awakening only briefly to eat. When awakened, they could interact in a relatively unimpaired fashion with the examiner, but soon fell asleep if not continuously stimulated.
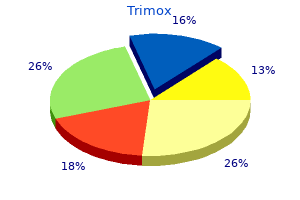
Some synkinesis and residual weakness will persist bacteria during pregnancy trimox 250mg on line, yet significant improvements in both function and appearance can be accomplished if the goals of reconstruction are kept in mind antibiotics you can't drink on purchase 250 mg trimox with mastercard. A skin graft retains an important role in oral cavity reconstruction and cutaneous facial defects. Complete immobilization of the graft in the early postoperative period is critical. Skin is the largest organ of the human body, representing 16% of the total body weight. Facial Plastic and Reconstructive Surgery 627 individual is termed an autogenous graft or autograft. Despite the development of sophisticated reconstructive methods utilized after ablative surgery, such as microvascular free flaps, much simpler approaches to reconstruction continue to be appropriate in many cases. Skin grafting in particular remains an excellent option for defects of the oral cavity, face, and scalp. N Anatomy and Physiology From superficial to deep, there are three layers of skin: the epidermis, the dermis, and the subcutaneous layer. The epidermis is further divided into the superficial stratum corneum (no nuclei) and the deeper basal layer. The dermis is further divided into the more superficial papillary dermis, and the deeper reticular dermis, which contains hair follicles and sebaceous glands. In the first stage, imbibition, the graft derives its nutrients from the underlying recipient bed. During the second stage, inosculation, preexisting blood vessels in both the graft and the recipient bed meet and form a network. Healing is completed by neovascularization, wherein new vessels form within the graft and grow into the underlying tissue. Skin grafts will "take" on most well-vascularized tissue, including granulation tissue, muscle, fat, perichondrium, and periosteum, and cancellous bone. Conversely, skin grafts will not survive on naked cortical bone or bare cartilage. N Indications Common settings for skin grafting in head and neck surgery include oral cavity defects after cancer resection, cutaneous defects of the face after lesion excision or trauma, closure of free flap donor sites (radial forearm, fibula, etc. N Operative Technique Split-Thickness Skin Graft G G the donor site of choice is the upper thigh (thick skin, relatively flat surface). Ensure the meticulous hemostasis of the recipient bed to prevent hematoma/loss of apposition. The skin graft is applied to the recipient site with the epidermis facing out then sutured into place with absorbable stitches, ensuring good apposition with the recipient bed. The edges of the graft are held with a skin hook, and the remainder of the graft is elevated from underlying fat using a knife or sharp scissors. G G G G G G Skin graft meshing: A skin graft may be meshed to provide coverage of a greater surface area at the recipient site, with expansion ratios generally ranging from 1:1 to 6:1. N Complications the major complication of skin grafting is partial or complete graft loss. Reasons for graft failure include hematoma, seroma, infection, and inadequate stabilization. Facial Plastic and Reconstructive Surgery 629 N Postoperative Care Feeding via a nasogastric feeding tube should be considered for oral cavity skin graft placement. A defect analysis should be done systematically to avoid untoward long-term results. Flap design must consider vectors of tension, resultant scars, and areas from which to recruit. Cutaneous defects can arise from a host of different causes, but skin cancer remains the most common etiology in the Caucasian population. Local facial flaps are widely used for defects that are too large for primary closure or second intention healing. They remain the workhorse for facial reconstruction and should be within the comfort level of all otolaryngologists. Examples of this would be the hairline, vermillion border of the lip, and nasal alar rim. These critical structures must remain undisturbed by scars as well as by flap tension.
The diagnosis can be established only after a thorough search for the usual causes of secondary pulmonary hypertension virus 2014 adults buy 250mg trimox with amex. The patients are usually young females between the age of 20 and 40 years antibiotics for sinus infection safe for breastfeeding cheapest generic trimox uk, or children around 5 years of age. Unrecognised thromboemboli or amniotic fluid emboli during pregnancy may play a role. There is a suggestion that primary pulmonary hypertension may be a form of collagen vascular disease. Pulmonary veno-occlusive disease characterised by fibrous obliteration of small pulmonary veins is believed to be responsible for some cases of primary pulmonary hypertension. Multiple emboli or thrombi Sickle cell disease Schistosomiasis Obliterative type. Chronic emphysema Chronic bronchitis Bronchiectasis Pulmonary tuberculosis Pneumoconiosis 3. In those residing at high altitude Pathologic obesity (Pickwickian disease) Upper airway disease such as tonsillar hypertrophy Neuromuscular diseases such as poliomyelitis Severe kyphoscoliosis. The vascular changes are similar in primary and secondary types and involve the entire arterial tree from the main pulmonary arteries down to the arterioles. Failure of defense mechanisms and presence of certain predisposing factors result in pneumonias. On the basis of the anatomic region of the lung parenchyma involved, pneumonias are traditionally classified into 3 main types: 1. Based on the clinical settings in which infection occurred, pneumonias are classified as under: 1. Two types of acute bacterial pneumonias are distinguished-lobar pneumonia and broncho(lobular-) pneumonia, each with distinct etiologic agent and morphologic changes. Pneumococcal pneumonia More than 90% of all lobar pneumonias are caused by Streptococcus pneumoniae, a lancet-shaped diplococcus. Staphylococcal pneumonia Staphylococcus aureus causes pneumonia by haematogenous spread of infection from another focus or after viral infections. Streptococcal pneumonia b-haemolytic streptococci may rarely cause pneumonia such as in children after measles or influenza, in severely debilitated elderly patients and in diabetics. However, these classic stages seen in untreated cases are found much less often nowadays due to early institution of antibiotic therapy and improved medical care. M/E Salient features are: i) Dilatation and congestion of the capillaries in the alveolar walls. The term hepatisation in pneumonia refers to liver-like consistency of the affected lobe on cut section. The cut surface of the involved lobe is airless, red-pink, dry, granular and has liver-like consistency. M/E Salient features are: i) the oedema fluid of the preceding stage is replaced by strands of fibrin. The cut surface is dry, granular and grey in appearance with liver-like consistency. G/A the previously solid fibrinous constituent is liquefied by enzymatic action, eventually restoring the normal aeration in the affected lobe. The cut surface is grey-red or dirty brown and frothy, yellow, creamy fluid can be expressed on pressing. M/E Salient features are: i) Macrophages are the predominant cells in the alveolar spaces, while neutrophils diminish in number. However, they may develop in neglected cases and in patients with impaired immunologic defenses. The major symptoms are: shaking chills, fever, malaise with pleuritic chest pain, dyspnoea and cough with expectoration which may be mucoid, purulent or even bloody. The common physical findings are fever, tachycardia, and tachypnoea, and sometimes cyanosis if the patient is severely hypoxaemic. G/A Bronchopneumonia is identified by patchy areas of red or grey consolidation affecting one or more lobes, frequently found bilaterally and more often involving the lower zones of the lungs due to gravitation of the secretions. On cut surface, these patchy consolidated lesions are dry, granular, firm, red or grey in colour, 3 to 4 cm in diameter, slightly elevated over the surface and are often centred around a bronchiole.
Retinoblastoma Retinoblastoma is a primary malignant intraocular neoplasm that arises from immature neuroepithelial cells of the developing retina (retinoblasts) bacteria bloom in aquarium cheap trimox 500mg visa. Some are present at birth antibiotics to treat bronchitis buy generic trimox online, and 501 occasionally, they have been identified by prenatal imaging. Pathologically, retinoblastoma is composed of small round neoplastic cells that invade and replace the normal retina. Individual tumor cells tend to have a large nucleus and disproportionately small amount of cytoplasm. Clinically retinoblastoma can affect one eye (usually unifocal) or both eyes (usually multifocally). Thus, children of such individuals have a nearly 50% chance of having the disease, and regular screening until the child has been shown by genetic testing not to be at risk is important in the early detection of tumors. In contrast, most individuals with unilateral, unifocal retinoblastoma do not have a germline mutation in the retinoblastoma gene and will not transmit the disease to their offspring. Recognized risk factors for occurrence of retinoblastoma include a positive family history and chromosome 13q deletion syndrome. Sequencing of the gene allows identification of carriers and hence more specific genetic counseling. The cumulative lifetime incidence of retinoblastoma has been estimated to be about 1 in 15,000 to 1 in 18,000 individuals in most Western countries. Larger discrete retinal tumors tend to develop intralesional foci of degenerative calcification, which usually can be detected by B-scan ultrasonography and computed tomography scanning. In eyes with extensive retinoblastoma, secondary iris neovascularization and neovascular glaucoma develop frequently. Retinoblastoma has a tendency to invade the optic disk and 502 extend into the orbital optic nerve, invade the choroid with possible hematogenous dissemination, and extend transsclerally to the orbit via scleral vascular and neural foramina into the orbit. Once retinoblastoma extends outside the eye, it tends to grow aggressively in the periocular tissues, extend via the optic nerve to the brain, and rapidly metastasize widely. Untreated, children with metastatic retinoblastoma rarely survive for more than 1 year. Two discrete intraretinal retinoblastoma tumors in the left eye of a child with bilateral retinoblastoma. The slightly larger superior tumor is more opaque while the smaller inferior tumor is more translucent. Multinodular macular intraretinal retinoblastoma tumor formed by coalescence of three distinct tumors. Retinoblastoma in children with a positive family history is frequently identified by screening examinations when the extent of intraocular disease is limited (ie, few tumors, small tumors, and no vitreous seeds). In most developed countries, the median age at initial diagnosis of retinoblastoma is about 12 months for bilateral cases and about 24 months for unilateral cases. In countries with limited health care services, the median age at detection of both groups tends to be substantially higher. White pupillary reflection (leukocoria) in each eye (more pronounced in the right eye) due to bilateral retinoblastoma. A number of systems (Reese-Ellsworth classification, Essen prognosis classification, International Classification of Intraocular Retinoblastoma) have been used over the years to categorize eyes with intraocular retinoblastoma into 504 ordinal categorical subgroups having distinct probabilities of disease eradication with ocular preservation using available therapies.
Purchase genuine trimox online. How to install a tile transition on floors: Schluter®-RENO-RAMP/-K.