"Buy cheap buspar, anxiety symptoms gas".
By: S. Goran, M.A., M.D.
Co-Director, Saint Louis University School of Medicine
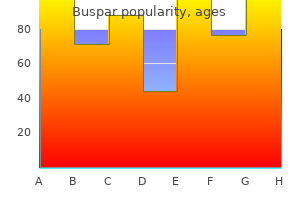
In the condition referred to as "apraxia of the eyelids anxiety depression buy buspar online from canada," the patients cannot close the eyelids voluntarily anxiety symptoms vs adhd symptoms generic buspar 5mg line, but they will still close reflexively in response to stimulation of the supraorbital branch of the trigeminal nerve (by a tap on the brow or bridge of the nose or by touching the cornea). Actually, the blink reflex is expressed by two electrical responses, one early and mainly ipsilateral (termed R1) and the other late and bilateral (R2). The late response (to a tap on the brow), which is lost in Parkinson disease and is enhanced in pseudobulbar palsy, utilizes large fiber bundles in the supraorbital nerves; the early response (corneal reflex) utilizes the small fiber bundles in the long ciliary nerves. Derangement of one of these reflexes or of the jaw jerk is found in 25 percent of patients with multiple sclerosis. In pseudobulbar palsy, tapping the tendinous insertions into the orbicularis oris elicits a buccal (trigeminofacial) reflex, which may spread to cause closure of the eyes. Facial Hemiatrophy (Parry-Romberg syndrome) An obscure disorder is the facial hemiatrophy of Romberg. It occurs mainly in females and is characterized by a disappearance of fat in the dermal and subcutaneous tissues on one or both sides of the face. In its advanced form, the affected side of the face is gaunt and the skin thin, wrinkled, and rather dark; the hair may turn white and fall out, and the sebaceous glands become atrophic; the muscles and bones are not involved as a rule. The condition is a form of lipodystrophy, but the localization within a myotome indicates the operation of some neural factor (possibly a growth factor) of unknown nature. A variegated coloration of the iris and a congenital oculosympathetic paralysis are found in some cases. Wilson and Hoxie have pointed out the frequent coexistence of facial asymmetry in adults with congenital or early-onset superior oblique palsy and compensatory head tilt or torticollis. If the peripheral facial paralysis has existed for some time and return of motor function has begun but is incomplete, a kind of contracture (in reality a continuous diffuse myokymic contraction) may appear. Attempts to move one group of facial muscles result in contraction of all of them (associated movements, or synkinesis). Spasms of facial muscles may develop and persist indefinitely, being initiated by every facial movement. With the passage of time, the corner of the mouth and even the tip of the nose may become pulled to the affected side. This is a special acquired form of hemifacial spasm, the more common variety of which is described below. If regenerating fibers originally connected with the orbicularis oculi become connected with the orbicularis oris, closure of the lids may cause a retraction of the corner of the mouth; or if visceromotor fibers originally innervating the salivary glands later come to innervate the lacrimal gland, anomalous tearing (crocodile tears) occurs whenever the patient salivates. Hemifacial Spasm the facial muscles on one side may be involved in painless irregular clonic contractions of varying degree (hemifacial spasm). This condition develops in the fifth and sixth decades, affects women more than men, and it usually proves to be due to a compressive lesion of the facial nerve, most often by a tortuous branch of the basilar artery that lies on the ventral surface of the pons and forms a loop under the proximal nerve. Less often the cause of compression is a basilar artery aneurysm, or an acoustic nerve tumor or meningioma. The spasm usually begins in the orbicularis oculi muscle and gradually spreads to other muscles on that side of the face, including the platysma. The paroxysm may be induced or aggravated by voluntary and reflexive movements of the face. Jannetta attributed all cases to a compression of the root of the facial nerve by an aberrant looped blood vessel. Microsurgical decompression of the root with the interposition of a pledget between the vessel and the root has relieved the facial spasm in most of his cases. These results have been corroborated by Barker and associates in a series of 705 patients followed postoperatively for an average period of 8 years; 84 percent achieved an excellent result. An even higher rate of benefit was obtained in a prospective series by Illingworth and colleagues (cure of 81 of 83 patients). The pathophysiology of the spasm is believed to be focal demyelination nerve root compression. The demyelinated axon is theorized to activating adjacent nerve fibers by ephaptic transmission ("artificial" synapse of Granit et al). Another possible source of the spasm is spontaneous ectopic excitation arising in injured fibers. Nielsen and Jannetta have shown that ephaptic transmission disappears after the nerve is decompressed. Treatment Surgical decompression of a vascular loop, which involves exploration of the posterior fossa, carries some small risk. Another complication has been deafness due to injury of the adjacent eighth nerve.
Long-term studies are sparse in veterinary medicine anxiety verses buy on line buspar, but these technologies offer the promise of higher doses to tumors relieve anxiety symptoms quickly buy buspar 10 mg mastercard, lower doses to normal structures, and fewer dosage fractions. Patients treated with palliative courses of radiation may not require computer-based planning depending on tumor size and location. The first attempt at surgical excision always offers the best opportunity to completely remove the tumor. Locally recurrent tumors often are more difficult to remove than the initial tumor because of more extensive involvement of normal tissues in the region and distortion of normal tissue planes by scar tissue. The usual objective of surgery is to obtain wide surgical margins in all directions surrounding the tumor, that is, to remove the tumor with a grossly visible intact cuff of surrounding normal tissue. There is no universally appropriate margin width, and adequate margins vary from tumor to tumor and location to Patient positioning during radiother- apy should attempt to exactly duplicate the patient position at the Tumor-Specific Radiation Considerations A variety of cancers are responsive to radiation therapy. These include brain tumors, nasal tumors, oral tumors, and tumors of the extremities and body. The necessary margin often depends in part on the type of tissues that are adjacent to the tumor. For example, fascial planes generally provide a good physical barrier to tumor growth, so that excision of an intact fascial plane below a tumor is an excellent way to optimize the chance of a complete excision. Subcutaneous fat is poorly resistant to tumor growth and should always be aggressively excised with the tumor mass. A marginal excision refers to ``shelling out' a tumor, or excising it just outside its pseudocapsule. Because the pseudocapsule often consists of compressed cancers cells, marginal excisions risk leaving microscopic quantities of tumor cells in the patient and are associated with higher rates of local recurrence than wide excisions. As a general rule, marginal excisions should be avoided unless postoperative radiation therapy is being considered. All excised tumors should be submitted for histopathologic examination and margin analysis. The accuracy of margin analyses can be optimized by inking the excised specimen to allow the pathologist to distinguish true surgical margins from artifactual margins created during tissue processing. Sutures may be placed in the surface of the excised specimen to guide the pathologist to areas of particular concern. Because pathology labs typically prepare only four or five slides from a given specimen, a report of complete margins does not necessarily imply that an excision was complete. A report of incomplete margins means the resection was histologically incomplete in at least one location. While overall recurrence rates are consistently greater for tumors with incomplete margins than for tumors with complete margins, owners should be aware that tumors with complete margins can recur locally and, conversely, many tumors with incomplete margins do not recur. Following a report of incomplete margins, options include close monitoring (if an appropriate re-excision will be feasible should local recurrence develop), immediate wide excision of the surgical scar, or postoperative radiation therapy. However, it is imperative for these patients to have periodic post-therapy examinations due to the possibility of recurrence, metastasis, new tumor development, or complications of initial therapy. Upon completion of initial therapy, patients are often restaged to determine extent of disease. Some tumors can take mo for the maximum treatment response to occur, so patience and ongoing supportive care is advisable. Partial response or stabilization of the growth of the primary tumor, leaving residual disease, may be the maximum post-therapy response seen. Maintenance Chemotherapy For many oncology cases, initial therapy is done to prolong survival even though it is not considered curative. Use of the latter two agents is justified by their antiangiogenic properties as well as their anti-proliferative effects. Pet owners should be prepared for repeat imaging and staging prior to final treatment decisions. Follow-Up Care Assessment of Response Guidelines have been developed to avoid arbitrary decisions in assessing therapeutic response. Responses must be viewed in context with the original intent of therapy, whether it be cure or palliation. The case study is not intended be prescriptive or to imply that the approach taken here is the only way to manage an osteosarcoma patient, nor is it intended to be used as a diagnostic tree. Practitioners interested in oncology are encouraged to research current diagnostics, chemotherapeutics, and modalities appropriate for each cancer patient as the best way of keeping current in this rapidly evolving field of veterinary medicine. The case history includes the rationale for ``decision points,' the interventions the clinician would make in appropriately treating the patient.
This is true also of adults with myxedema anxiety or depression discount 10 mg buspar with amex, Addison disease anxiety symptoms even on medication buy generic buspar 10 mg, chronic liver disease, and pneumonia. Acute poisoning may also occur in addicts who are unaware that available opioids vary greatly in potency and that tolerance for opioids declines quickly after the withdrawal of the drug; upon resumption of the habit, a formerly well-tolerated dose can be fatal. Varying degrees of unresponsiveness, shallow respirations, slow respiratory rate. In the most advanced stage, the pupils dilate, the skin and mucous membranes become cyanotic, and the circulation fails. The immediate cause of death is usually respiratory depression, with consequent asphyxia. Patients who suffer a cardiorespiratory arrest are sometimes left with all the known residua of anoxic encephalopathy. Mild degrees of intoxication are revealed by anorexia, nausea, vomiting, constipation, and loss of sexual interest. Treatment of Overdose this consists of the administration of naloxone (Narcan), or the longer acting nalmefene, both specific antidotes to the opiates and also to the synthetic analgesics. In cases of opioid poisoning, the improvements in circulation and respiration and reversal of miosis are usually dramatic. In fact, failure of naloxone to produce such a response should cast doubt on the diagnosis of opioid intoxication. If an adequate respiratory and pupillary response to naloxone is obtained, the patient should nonetheless be observed for up to 24 h and further doses of naloxone (50 percent higher than the ones previously found effective) can be given intramuscularly as often as necessary. Naloxone has less direct effect on consciousness, however, and the patient may remain drowsy for many hours. Although nalmefene has a plasma halflife of 11 h, compared to 60-90 min for naloxone, it has no clear advantage in emergency practice. This procedure may be efficacious many hours after ingestion, since one of the toxic effects of opioids is pylorospasm and ileus, which causes much of the drug to be retained in the stomach. Once the patient regains consciousness, complaints such as pruritus, sneezing, tearing, piloerection, diffuse body pains, yawning, and diarrhea may appear. These are the recognizable symptoms of the opioid abstinence, or withdrawal, syndrome, described later. An antidote therefore must be used with great caution in an addict who has taken an overdose of opioid, because in this circumstance it may precipitate withdrawal phenomena. Nausea and severe abdominal pain, due presumably to pancreatitis (from spasm of the sphincter of Oddi), are other troublesome symptoms of opiate use or withdrawal. These persons, after several repetitions, recognize a "high," despite the subsequent recurrence of unpleasant, or dysphoric, symptoms (nausea, vomiting, and faintness as the drug effect wanes). Regardless of how one characterizes the state of mind that is produced by episodic injection of the drug, the individual quickly discovers the need to increase the dose in order to obtain the original effects (tolerance). Although the initial effects may not be fully recaptured, the progressively increasing dose of the drug does relieve the discomfort that arises as the effects of each injection wear off. In this way a new pharmacogenically induced need is developed, and the use of opioids becomes self-perpetuating. At the same time a marked degree of tolerance is produced, so that enormous amounts of drugs. The pharmacologic criteria of addiction, as indicated in the chapter on alcoholism, are tolerance and physical dependence. The latter refers to the symptoms and signs that become manifest when the drug is withdrawn following a period of continued use. These symptoms and signs constitute a specific clinical state, termed the abstinence or withdrawal syndrome (see later). The mechanisms that underlie the development of tolerance and physical dependence are not fully understood. However, it is known that opioids activate an opioid antinociceptive system (enkephalins, dynorphins, endorphins), which are opioid receptors and are located at many different levels of the nervous system (these are described in Chap.
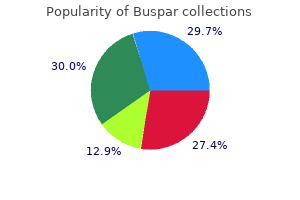
Safety and effectiveness in pediatric patients below the age of 12 has not been established performance anxiety quality buspar 10 mg. Other reported clinical experience has not identified differences in responses between the elderly and younger patients anxiety joint pain buy cheap buspar 10 mg on-line. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and concomitant disease or other drug therapy. However, adverse reaction information from clinical trials provides a basis for identifying the adverse events that appear to be related to drug use. Autoimmune conditions: polyarthralgia, pericarditis, exacerbation of systemic lupus, pulmonary infiltrates with eosinophilia, transient lupus-like syndrome. Central nervous system: pseudotumor cerebri, bulging fontanels in infants, decreased hearing. Preliminary studies suggest that use of minocycline may have deleterious effects on human spermatogenesis (see Carcinogenesis, Mutagenesis, Impairment of Fertility section). Minocycline is not removed in significant quantities by hemodialysis or peritoneal dialysis. Patent 5,908,838 and patent pending May 2006 46010-13A botulinum toXin tyPe a in the treatment oF Primary FoCal sCalP hyPerhiDrosis: a Case rePort Jami Reaves, D. Primary focal hyperhidrosis is an idiopathic disorder of excessive sweating of the axillae, palms, soles or craniofacial region. While there is strong evidence supporting the available treatments for axillary and palmo-plantar hyperhidrosis, there has been limited study in the management of craniofacial hyperhidrosis. A 65-year-old female with a history of well-controlled hypertension, hypothyroidism, and urge urinary incontinence presented to our continuity clinic with a chief complaint of "excess scalp sweating" that occurred almost daily for "many years. She also noted that her symptoms lasted longer than the "hot flashes" of peri-menopause, often for many hours. She denied relation of symptoms to emotion, exercise or foods; associated palpitations, abdominal cramping, nausea, vomiting or diarrhea; shortness of breath; headache; visual change; lethargy; weight loss; or weakness. On physical examination, the patient was a well-appearing, mildly overweight female with obvious hyperhidrosis involving the scalp and forehead. Other than incidental solar lentigines and seborrheic keratoses, the rest of her physical exam was unremarkable. Laboratory evaluation to rule out pheochromocytoma was also unexceptional (Table I). Since the patient had already failed topical aluminum chloride 10% solution, her treatment options included simple avoidance of triggers, oral or topical anticholinergics, or sympathectomy. The patient had read an article about the treatment of excess perspiration of the axillae with Botox and asked if that would be effective for her scalp. Botulinum toxin type A has been used with success in axillary, palmo-plantar, gustatory and even frontal hyperhidrosis, but to our knowledge had never been used for primary scalp hyperhidrosis. As botulinum toxin type A has been used safely and effectively via intramuscular injections of the temporal and occipital scalp in the treatment of migraine and tension headache, it was felt to be safe to use for intradermal injection for scalp hyperhidrosis in those locations. After proper patient consent was obtained, 20 units of botulinum toxin type A (dilution of 100 units with 3 cc normal saline) was injected in a scattered pattern in the superficial dermis of the right temporal scalp as a testpatch over an area of 20 cm2 via a 30-gauge hypodermic needle. No further treatment was offered at that office visit, as response times to botulinum toxin type A have been reported to take up to three to four weeks after initial treatment of frontal hyperhidrosis and headache disorders. At that time, the patient had noticed decreased sweating on the right frontal scalp compared to her left and had noted no adverse side effects. Discussion There are three major sweat glands in humans: eccrine, apocrine and apoeccrine glands. They have a generalized distribution and are under emotional, thermal and neural influence. Innervation of the eccrine glands is provided by post-ganglionic sympathetic fibers that have acetylcholine as their principal terminal neurotransmitter; these fibers are controlled by the hypothalamic sweat center. Hyperhidrosis may be primary or secondary to neural dysfunction, local heat, drugs, or changes in blood flow to sweat glands. Intradermal botulinum toxin type A is a relatively new option in the treatment of primary focal hyperhidrosis, with significant data supporting its efficacy and safety. They both block neuromuscular motor transmission by binding to receptor sites on motor nerve terminals and inhibiting the release of acetylcholine.
5mg buspar overnight delivery. Separation anxiety.