"Order 200mg bexovid visa, hiv infection rates in poland".
By: C. Denpok, M.A., M.D.
Co-Director, University of New Mexico School of Medicine
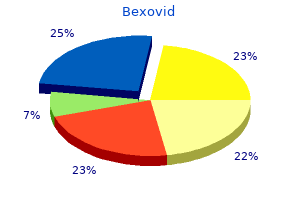
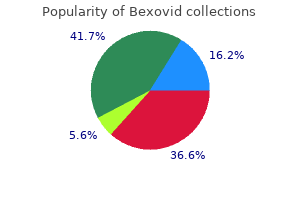
Of the remaining 37 antiviral universal best 200 mg bexovid,169 (86 antiviral elixir cheap bexovid 200 mg visa,439 49,270), it is unknown how many will meet the work or other requirements due to a lack of data related to this population. For purposes of this analysis, it is assumed an additional 40 percent, or 14,868 (37,169 x 40. Therefore, it is assumed approximately 22,301 (37,169 14,868) will not meet requirements, be dis-enrolled and will appeal the dis-enrollment decision. It is assumed appeals will not exceed 2017 numbers of 138,486 with the additional disenrollments; therefore any increase in expenditures can be accommodated within existing resources. Case Management Costs: Based on projections from other states for the per-member per-month (pmpm) case management of the work requirement, these costs are dependent on current programs that are in place and the degree of assistance provided enrollees. It is assumed that at a minimum, TennCare will incur a $100 pmpm case management cost. The total case management costs are based on the total work requirement population that is not currently working of 37,169. The estimated increase in expenditures will be $44,602,800 (37,169 x $100 x 12 months). Staffing: TennCare will need two program administrator positions to assist in the implementation and oversight of the program. Savings: There will be savings from TennCare enrollees being dis-enrolled from the program from not meeting the work requirements or for reaching an income level in which they no longer qualify for TennCare assistance. It is also unknown as to the timeframe in which a dis-enrolled individual is able to prove compliance with the new requirements and re-enroll into the program. The 2017 medical and pharmacy costs for someone enrolled in TennCare is $380 pmpm. Should 10 percent of the 37,169 enrollee population be dis-enrolled for at least a six month period, the estimated savings would be $10,704,672 [(37,169 x 10. Work requirements in welfare programs in the past have had different goals of strengthening self-esteem and providing a ladder to economic progress, versus improving health. This brief examines literature on the relationship between work and health and analyzes the implications of this research in the context of Medicaid work requirements. We review literature cited in policy documents, as well as additional studies identified through a search of academic papers and policy evaluation reports, focusing primarily on systematic reviews and meta-analyses. There is limited evidence on the effect of employment on health, with some studies showing a positive effect of work on health yet others showing no relationship or isolated effects. There is strong evidence of an association between unemployment and poorer health outcomes, but authors caution against using these findings to infer that the opposite relationship (work causing improved health) exists. While unemployment is almost universally a negative experience and thus linked to poor outcomes, especially poor mental health outcomes, employment may be positive or negative, depending on the nature of the job. Further, most studies note major limitations in our ability to draw broad conclusions on health and work, including: o o Job availability and quality are important modifiers in how work affects health; transition from unemployment to poor quality or unstable employment options can be detrimental to health. Studies note several caveats to and implications of the research on work and health that are particularly relevant to work requirements in Medicaid. For example: o the work-health relationship may differ for the Medicaid population compared to the broader populations studied in the literature, as Medicaid enrollees report worse health than the general population and face significant challenges related to social determinants of health. Work or volunteering to fulfill a requirement may produce different health effects than work or volunteer activities studied in existing literature. Loss of Medicaid coverage under work requirements could negatively impact health care access and outcomes, as well as exacerbate health disparities. However, the court also noted that plaintiffs and their amici assert that proclaimed health benefits of employment are unsupported by substantial evidence. Thus, there is likely to be ongoing debate and policy discussion over whether work requirements will further the aims of Medicaid. To address whether work will further the aims of Medicaid, we examine the literature on the relationship between work and health and analyze the implications of this research in the context of Medicaid work requirements. Due to the large number of studies in this field spanning decades, this literature review focuses primarily (although not exclusively) on findings from other literature or systematic reviews rather than individual studies on these topics. We drew on studies cited in policy documents on work requirements in Medicaid, results of keyword searches of PubMed and other academic health/social policy search engines, and snowballing through searches of reference lists in previously pulled papers. In total, we reviewed more than 50 sources, the vast majority of which were published academic studies or program evaluations and most of which are reviews of multiple studies themselves.
For these populations antivirus windows server 2008 discount 200 mg bexovid, social conditions such as homelessness or housing instability seriously interfere with personal energy hiv infection listings effective bexovid 200 mg, storage of medication and testing equipment, limited food choices and money necessary to manage their diabetes (Keene, et al. Incentives that target disadvantaged populations, particularly for behavioral change, can be a positive way to decrease unfair inequality in health. They are, however, ethically problematic if individuals cannot afford to decline an incentive even if they would not consider it in their best interest, or if the incentive sends a message of unequal social status, is stigmatizing or marks these populations as irresponsible (Voight, 2017). Is the system not fairly allocating resources to prevent or decrease chronic illness? Is it not producing better outcomes of importance to patients and asking families and patients to do too much? The evidence that is available and cited above suggests some indifference within the health care system to adequately address important elements of chronic disease care. While the Hastings Center Report quote at the beginning of this paper suggests that society should decide how those with chronic disease should be treated, those designing and operating the health system and those producing its scientific base have professional responsibilities to provide care that is efficacious and safe, and should reflect the increasing patient-centeredness evident in at least some recent public policy. If the health care system is a potential wrongdoer, are the health professionals that form the workforce complicit in areas of essential care, such as chronic disease, that are systematically underdeveloped? Do health professionals have a duty to challenge health system policy and practice contributing to this underdevelopment? A claim of complicity is judged by how proximate, reversible or frequent the contribution was and whether the wrongdoing purpose was shared (Lepore & Goodin, 2017). Because there is little direct evidence that those designing and providing care to patients with chronic disease intended to deliver suboptimal care to persons trying to self-manage, strong complicity is unlikely. An implicit authority seems to have set priorities favoring acute care, making these preferences seem normal and inconsequential accompanied by a diffusion of responsibility (Passini, 2017) that renders no one responsible for the lifelong care that will optimally manage the disease but also sustain or restore optimal functioning and well-being. Listen to our language and practices: People with chronic disease could have avoided it if they had chosen to live differently. How do we approach the overwhelming need for patients to do much of the work to manage chronic disease while assuring they are competent to do so and are supported? Ethical Issues in Responding to Chronic Diseases 121 · Invest in common definitions and research that will systematize the evidence base and be viewed as fair. A review of the few studies that do exist found that integrated psychiatric and medical interventions have been successful and should be extended. But the fact that these studies used more than 70 different measurement instruments precluded a meta-analysis of the accumulated findings (Whiteman et al. Treat chronic disease as itself a health disparity as well as for some groups within it. Use interventions and measures that directly target disparities; include equity as a domain of performance measurement; use value-based payment; and build partnerships to address factors outside the direct control of the health care system (Anderson, et al. Although theories of justice and their indicators, identified earlier in the paper, are idealizations, they offer perspective about what is right. Heavy focus on biological outcome measures confirms a commitment to a narrow medical view. If used, the capability approach attends to those most in need and supports capabilities needed to be learned for normal functioning. Perhaps developing a dedicated service of nurses with documented skills and wide availability to all persons with chronic diseases is a start. This service should also document patient needs, test tools and become an advisory unit for development of the evidence base that is necessary to professionalize the service. Liaison with social and legal services should document social and environmental factors contributing to chronic disease and test policy and advocacy approaches to reverse those practices detrimental to health. Shifting of both blame and responsibility to patients, failure to study and establish approaches that meet their needs, and tolerance of poor research methodology have all been described. All of these issues are correctable, but apparently not in the current health care system and perhaps through the political institutions setting terms for its structure and function. This leads to the question: What is needed for a representative deliberation to reach some level of consensus which has been evading us since it was documented in the 1980s by a Hastings Center report (Jennings, et al. There still appears to be a dramatic imbalance of power between patients and the health care system, modest movement from the normative framework of patient responsibility for lifestyle control and compliance with the medical regimen, and strong preference for biological over social outcomes. The history of our collective moral learning requires that we reject some of our current practice and its structure, which we have come to believe is wrong (Appiah, 2017). We should know now what changes are feasible, given the social structures in which they are embedded, understanding that the ideal may not yet be feasible.
Buy bexovid 200mg free shipping. HIV / AIDS - Structure Replication Symptoms Transmission Diagnosis and Treatment.
Wintergreen. Bexovid.
- How does Wintergreen work?
- Are there any interactions with medications?
- Headache, minor aches and pains, stomachache, gas (flatulence), fever, kidney problems, asthma, nerve pain, gout, arthritis, menstrual period pains, arthritis-like pain (rheumatism), and other conditions.
- Are there safety concerns?
- What is Wintergreen?
- Dosing considerations for Wintergreen.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96762
Accrued knowledge of everyday tasks antiviral fruit purchase 200 mg bexovid visa, such as grocery prices hiv infection stories purchase bexovid 200mg with mastercard, can help older adults to make better decisions than young adults (Tentori, Osheron, Hasher, & May, 2001). Research has shown that older adults are less able to selectively focus on information while ignoring distractors (Jefferies et al. Other studies have also found that older adults have greater difficulty shifting their attention between objects or locations (Tales, Muir, Bayer, & Snowden, 2002). Researchers have studied cognition in the context of several different everyday activities. Although older adults often have more years of driving experience, cognitive declines related to reaction time or attentional processes may pose limitations under certain circumstances (Park & Gutchess, 2000). In contrast, research on interpersonal problem solving 401 suggested that older adults use more effective strategies than younger adults to navigate through social and emotional problems (Blanchard-Fields, 2007). In the context of work, researchers rarely find that older individuals perform poorer on the job (Park & Gutchess, 2000). Similar to everyday problem solving, older workers may develop more efficient strategies and rely on expertise to compensate for cognitive decline. Problem Solving: Problem solving tasks that require processing non-meaningful information quickly (a kind of task that might be part of a laboratory experiment on mental processes) declines with age. Older adults resolve everyday problems by relying on input from others, such as family and friends. They are also less likely than younger adults to delay making decisions on important matters, such as medical care (Strough, Hicks, Swenson, Cheng & Barnes, 2003; Meegan & Berg, 2002). The processing speed theory, proposed by Salthouse (1996, 2004), suggests that as the nervous system slows with advanced age our ability to process information declines. This slowing of processing speed may explain age differences on many different cognitive tasks. For instance, as we age, working memory becomes less efficient (Craik & Bialystok, 2006). Yet, when given sufficient time older adults perform as competently as do young adults (Salthouse, 1996). Thus, when speed is not imperative to the task healthy older adults do not show cognitive declines. In contrast, inhibition theory argues that older adults have difficulty with inhibitory functioning, or the ability to focus on certain information while suppressing attention to less pertinent information tasks (Hasher & Zacks, 1988). In directed forgetting people are asked to forget or ignore some information, but not other information. For example, you might be asked to memorize a list of words but are then told that the researcher made a mistake and gave you the wrong list and asks you to "forget" this list. While most people do well at forgetting the first list, older adults are more likely to recall more words from the "forget-to-recall" list than are younger adults (Andrйs, Van der Linden, & Parmentier, 2004). Cognitive losses exaggerated: While there are information processing losses in late adulthood, overall loss has been exaggerated (Garrett, 2015). One explanation is that the type of tasks that people are tested on tend to be meaningless. For example, older individuals are not motivated to remember a random list of words in a study, but they are motivated for more meaningful material related to their life, and consequently perform better on those tests. When age comparisons occur longitudinally, however, the amount of loss diminishes (Schaie, 1994). When older adults practiced skills, they performed as well as they had previously. In fact, Salthouse and Babcock (1991) demonstrated that processing speed accounted for all but 1% of age-related differences in working memory when testing individuals from 18 to 82. Longitudinal research has proposed that deficits in sensory functioning explain age differences in a variety of cognitive abilities (Baltes & Lindenberger, 1997). Not surprisingly, more years of education, and subsequently higher income, are associated with higher cognitive level and slower cognitive decline (Zahodne, Stern, & Manly, 2015). Intelligence and Wisdom When looking at scores on traditional intelligence tests, tasks measuring verbal skills show minimal or no age-related declines, while scores on performance tests, which measure solving problems quickly, decline with age (Botwinick, 1984).
Self-management behaviors should be incorporated into the treatment plan at all stages of chronic kidney disease hiv infection and diarrhea safe 200 mg bexovid. Patients with chronic kidney disease should be referred to a specialist for consultation and co-management if the clinical action plan cannot be prepared antiviral skin ointment buy 200 mg bexovid overnight delivery, the prescribed evaluation of the patient cannot be carried out, or the recommended treatment cannot be carried out. An action plan for patients with chronic kidney disease also requires interventions during the earlier stages of kidney disease, irrespective of the cause of kidney disease. Definition and Classification 67 ing progression of kidney disease, cardiovascular disease risk reduction, preventing and treating complications of chronic kidney disease, and preparation for kidney replacement therapy. The definitive diagnosis of the type of kidney disease is based on biopsy or imaging studies. Biopsy and invasive imaging procedures are associated with a risk, albeit usually small, of serious complications. Therefore, these procedures are often avoided unless a definitive diagnosis would change either the treatment or prognosis. In most patients, well-defined clinical presentations and causal factors provide a sufficient basis to assign a diagnosis of chronic kidney disease. An approach to diagnosis, based on concepts elaborated on in this report, is given in Part 9. Diabetic kidney disease is a type of glomerular disease, but it is singled out here because it is the largest single cause of kidney failure. Because of the higher prevalence of type 2 diabetes, it is the more common cause of diabetic kidney disease. The clinical features, natural history and treatment for diabetic kidney disease are well known because it has been the subject of numerous epidemiological studies and clinical trials. Clinical trials have established a number of effective treatments to slow the development and progression of diabetic kidney disease, including strict glycemic control, angiotensinconverting enzyme inhibitors and angiotensin receptor blockers, blood pressure control, and perhaps dietary protein restriction. A variety of diseases, including other glomerular diseases, vascular diseases, tubulointerstitial diseases, and cystic diseases, are often grouped together under the label ``nondiabetic kidney diseases' for the purpose of epidemiological studies and clinical trials. Amongst these, hypertensive nephrosclerosis and glomerular diseases are the second and third most common causes of kidney failure. The various diseases in this group differ widely based on history, clinical presentation, risk for progression, and response to treatment. Differentiation among the diseases can be difficult, often requiring kidney biopsy or invasive imaging studies. An approach to diagnosis, based on the history, and a review of clinical presentations of chronic kidney disease, are given in Part 9. Specific therapies are available to reverse abnormalities in structure and function for some types of chronic kidney disease: for example, immunosuppressive medications for autoimmune glomerular diseases, antibiotics for urinary tract infections, removal of urinary stones, relief of obstruction, and cessation of toxic drugs. A thorough search for ``reversible causes' of decreased kidney function should be carried out in each patient with chronic kidney disease. Kidney disease in the transplant is probably the fourth largest cause of kidney failure. Definition and Classification 69 Both immunologic and non-immunologic factors appear to play an important role. The most common causes are chronic rejection, toxicity due to cyclosporine or tacrolimus, recurrent disease, and transplant glomerulopathy. In addition, differential diagnosis includes all the diseases that can occur in the native kidney. For a variety of reasons, especially the ease and safety of kidney biopsy, there is generally a much lower threshold for performing invasive procedures to establish a definitive diagnosis in kidney transplant recipients. Comorbidity is defined as conditions other than the primary disease (in this case, chronic kidney disease). Complications of chronic kidney disease, such as hypertension, anemia, malnutrition, bone disease and neuropathy, are not considered as comorbid conditions. This is particularly important for patients with diabetes and high blood pressure, the leading causes of chronic kidney disease and cardiovascular disease in the United States. Unrelated diseases, which may lead to impairments of functioning and well-being but do not affect the course of chronic kidney disease. Cardiovascular disease is singled out from among the possible comorbid conditions to emphasize its complex relationship with chronic kidney disease, and its importance as a preventable cause of morbidity and mortality in patients with chronic kidney disease.